- To Change Your Mind - Details Matter
ADHD and TBI: Hopes, Cautions, Medication Protocols: CorePsych Radio
ADHD and Bipolar: Controversy Explored at CorePsych Radio
April 8, 2009ADHD Medications: Use The Therapeutic Window – CorePsych Radio
April 22, 2009ADHD and TBI: Hopes, Cautions, Medication Protocols
on CorePsych Radio this Thursday at 4PM EDT, 1PM PDT
Program Notes here: Download the pdf for ADHD and TBI
Seeing is Believing:
After having seen thousands of SPECT brain scans, I can report with certainty that Traumatic Brain Injury TBI is often missed in the ADHD differential, and is more frequently found than expected. TBI is where SPECT proves most useful to assess either or both ADHD and TBI as well as comorbid mood disorder.
- From “mild post concussive syndrome,” to “no overt symptoms” that appear brain related, brain injury can is often overlooked.
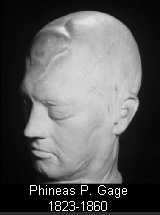
- Remember Phineas Gage 1848: You don’t have to be knocked unconscious.
- Often the patient doesn’t remember the injury until they actually see their brain in the SPECT review process.
- Brain injury does make a big difference in the process of adjusting ADHD meds. Those with TBI are very sensitive to any medical intervention, especially stimulant meds, and indeed any meds for any comorbid conditions, such as antidepressants for depression.
- A different, more careful, attitude with TBI medication treatment objectives can significantly improve outcomes. TBI can often have associated ADHD problems, and we often use augmentation with stimulant medications after temporal lobe dysregulation is adequately addressed.
In the previous program on Bipolar Disorder, we reviewed the importance of making the differential diagnosis of Traumatic Brain Injury [TBI] in mood disorders. If TBI is overlooked, the stimulant meds simply don’t work effectively, and they often make the patient worse.
Seven Tips on TBI and ADHD:
- Ask about head injury: Clinical evidence and the scientific literature contain numerous references regarding ADHD symptoms occurring simultaneously with brain injury. Often brain injury will aggravate a pre-existing ADHD as one or multiple injuries can draw down on the brain reserve – it’s ability to compensate and regenerate
- CAT and MRI findings: Often miss functional aspects of TBI and cannot differentiate ADHD: Consider having functional brain imaging to see the problems. Brain injury injures function more clearly than it shows anatomically. SPECT and PET are functional imaging processes to evaluate the locality of the brain dysfunction.
- ADHD Meds aggravate comorbid TBI: – Unless the meds are set up in sequence with full regard for the specific brain issues present in the brain injury. Numerous citations in the literature agree that stimulants may be used with brain injury, but they must be used with caution. [Vyvanse water titration.]
- Functional SPECT imaging to set the plan: SPECT will help establish an order to starting medications – temporal lobes can become significantly dysregulated with injury, and stimulant meds aggravate temporal lobe problems. Start with temporal interventions first.
- Dosing strategies for ADHD and TBI: Always go lower and slower with dosing in situations with coexisting ADHD and brain injury. Start with antiepileptics first and regulate moods, then next to the stimulants if depression is not associated.
- Atypical reaction to stimulants – suspect TBI: This is not the way to make the diagnosis of brain injury, but for various reasons, from denial to accommodation, the TBI diagnosis is missed at first. If TBI is missed, the stimulant meds will cause profound reactions.
- Brain reserve: Enhanced with stimulant medication, encouraging less injury. – Less re-injury, more healing. Antidepressants have shown specific BDNF increases in rats. TBI with ADHD is the place for neurotransmitter precursor testing to actually heal brain and increase NT efficiency. Simple DA reuptake inhibitors don’t adequately cover the long -term recovery process.
—————-
Addendum 2013 – More Is Available
We're still providing SPECT imaging readings here at CorePsych, including SPECT Second Opinions for individuals who've received SPECT evaluations from other providers.
We have, however considerably evolved to provide additional significant evidence through IgG immune testing, TMA Tissue Mineral Analysis, and Neurotransmitter Testing – for those treated for Traumatic Brain Injury with less than satisfactory responses to meds or to supplements. Our edge here: Evolved neuroscientific measurement strategies that compliment testing already completed – and a firmly comprehensive review that combines medication and cellular neurophysiological understandings.
—————-
See ya there!
cp
Related articles by Zemanta








34 Comments
when I was a about five, I fell off the top of a metal jungle gym, and landed head first on the bottom bar of the jungle gym, right on the ridge between the eyebrows. received a long column of stitches. have a high iq but have always been an extreme under achiever- very lethargic and unmotivated. no real drive or ambition. have a great deal of anxiety for which I’ve been taking lexapro for last ten years. been taking Ritalin for last few years. helps at work, but often feel like its making me euphoric and compulsive. my wife says I pay too much attention to my own interests and not enough to the needs of my family. this makes me worry that I’m over focusing and have a problem differentiating what’s important from what’s not. I just read this can be a problem of too much dopamine. but my psychiatrist says I’m on a relatively low dose of Ritalin- 30 mg sr – so this confused me until I read what u said about tbi having sensitivity too meds. I’m desperate to get my life on track. hope you can provide some insight and guidance. thx -mr
Matt,
Low dosage with past TBI is relative, and often a small dose will do the trick. Honestly I also, as you might have noticed, prefer Vyvanse over Ritalin because you simply also might be out of meds by the time you get home. Duration, DOE, and the Therapeutic Window covered repeatedly on these pages might further answer some questions regarding what you are experiencing with family and meds.
cp
PS Lethargy and unmotivated frequently are associated with serotonin challenges, and can be paradoxically aggravated by dopamine products… see the “Depression and ADHD” video over on my channel at YouTube.
thanks! watched the video and definitely have experienced a little of the see saw effect. just downloaded your medication rules book. do you think I should get tested for tbi, or is it reasonable to assume that I had at least a mild tbi? or does it even matter? thx mr
Matt,
Likely had a real TBI, and probably would show on SPECT, but it won’t change the treatment if you spend 3500$. What will change your treatment, if the meds thing reaches a counterproductive plateau, is a combo of neurotransmitter, IgG and trace element testing for the molecular and cellular details.
cp
i in two thousand and three had a severe brain injury temporary shunt feeding tube respirator life support half paralyzed and 6 sliipped buldging disc in my neck i had such bad ptsd i was drinking and smoking pot every day and was told not two i went to kessler institution transitions of LI and lakeview of new hamshiree i made alot of mistakes due two impulse controll disorde an actede out of sourts and wound op in 28 phyc hospitals due two my injury and irradic drug use ijust recently was living up state and was taking inderol 10 mgs twice aday 20mgs lexapro 1 in am and pm 20 mg adderall xr 3 times daily 1500 mgs depicote xr at pm unfortunitely i had came back too moms in li and missed dr appt upstate got temporary meds till see my phyciast in late jan im seeing a therapist next week theese are the meds i a am am on know 10 mgs propanolal in am and pm 20 mgs lexapro in am 10 mgs ritalin er 3 times daily which isnt really helping like the adderal was 1 mg klonipan am and pm and 1500 depikote er pm but since my medicines changed ifeel anxiety tirerd nerveous i also get slightly paranoid what is your advice of med changes i was also on arricept and it worked well for short term memory
Movinon,
Yours is a very complicated situation, beyond just an internet shot in the dark without time and careful adjustment of meds.
Your very best bet is first the basic: do what your doc says and if you have a prob, tell the doc.
Next: Every TBI I have seen has significant neurotransmitter imbalances that require review. Measure them, look at any other less obvious challenges, like basic metabolic challenges that interfere with brain healing: e.g. IgG testing
Substance abuse with TBI is very difficult to treat because the patient remains at once sensitive to med changes, but confounds the psych meds with the street drugs that unwind any good efforts your doc is making.
cp
Dr. Parker,
My step son choked on a cheery seed when he was three years old. The EMT’s could not revive him at home and on most of the drive to the hospital. Thankfully, they were able to revive him as they arrived. My wife describes a change in behavior after the incident from a passive and docile child to aggressive, compulsive, and lacking of apathy.
Does a lack of oxygen to the brain for an extended period of time fall under the TBI diagnosis?
He was diagnosed with ADHD at age 6 and prescribed a stimulant of which he still takes at age 17. TBI was not taken into account.
The prescriptions have changed over the years, but unfortunately not his behavior at home and school. We’ve placed him in private school, in the hopes that a smaller class room would provided more personal attention to his needs. The school has now denied his return due to his behavior. We’re concerned that he will not be ready to be on his own after high school.
If he does have TBI and ADHD, what path should we take for treatment and behavioral modification other than stimulants?
Dan,
TBI is a possibility if you son was indeed hypoxic for a period of time. Yes, that can fall under the TBI diagnosis and does require a more careful review, more careful attention to the medication strategies – as well as the nutritional support strategies.
A SPECT scan will tell you more, with specific neurophysiologic implications based upon the area of the brain challenged. My own preference, and much more cost effective Neuroscience neurotransmitter review and, depending upon the response to neurotransmitter precursors targeted by that testing, Metametrix Triad panel [see that same page just below NeuroScience] to see the underlying nutritional tone for specific supplements.
And always consider Neurofeedback in these presentations – starting with a good QEEG.
cp
My son Matt, 15, sustained a L2 concussion 18 months ago in a helmet to helmet hit during football practice. He never lost consciousness, but he suffered with blurred vision, slurred speach, walking issues(had to watch his feet to walk), and procedural memory problems, which lasted for a few months. He had a clear xray and MRI. We have been to a brain injury doc, who recommended a neuro psych exam. That revealed some right hemisphere impairment,that the psychologist felt was due to his injury. The brain injury doc. felt that cognitive behavior therapy would be a help. Our insurance company specifically excludes this type of therapy. To complicate matters, he has ADHD, and a learning disability which he has been medicated for since he was 6. Currently he is pulling his hair out to the point where he has a bald spot at the hair line, he is struggling in school, and seems generally unable to follow any multi step directions, even when simple. He has trouble orgainizing even the easiest of tasks. How do I go about finding an expert in my area? Can you recommend someone? We don’t want to waste any more time in not getting the best help for him. Where do I start?
Kathy,
Complex problem, especially depending on where you live. If you are in Possum Hollow, fill up the gas tank as you will be unlikely to find someone in town. Having said that I would start with a pediatric neurologist who specializes in ADHD. The hair pulling is clearly indicative of neurotransmitter imbalance, and with complex cases I always measure before I shoot.
cp
I was in a MVA “rear-ended” in April 2009 I was only dazed from hitting the back of my head on the window, I started having Migraines 3 day’s after the accident my PCM sent me for MRI with contrast and referred me to neuro. The Neuro Doc told me I had white matter Lesions on the left Occipital lobe, frontal lobe and Brain stem, I also have a black spot in my central vision in right eye. I am in the Military and they will not DX me with TBI they have DX me with ADHD and learning disorder,nos- I am 41 years old and have never had any of these problems. I also have trouble swallowing, memory, sleeping , fatigue, depression, migraines 2x a week, head ache every day, stiff neck and its been almost 1 year since the accident. I need to know what I need to do to get well because here im not getting any help as I was denied treatment at the TBI Clinic because my injury was not Combat related. fighting uphill battle.
Tim,
1. Find a doc that gets it. There are many very good neuros that can jump on your symptoms [and, yes, they sound quite medical] – and will stand up with you. Fire the shirkers without a second thot, and seek the seekers. Seekers are all over the place, you just have to look a bit harder.
2. Try these guys: Defense and Veterans Brain Injury Center – they are very familiar with stories like this, and even tho you are Active Duty, just keep taking it higher. Try your GMO tomorrow and start by asking the nurse/corpsman for the doc that will stand to.
3. Go private pay if you have to, you only go around once.
cp
Dear C Parker,
Would a TBI 22 years ago be the explanation for all the issues I have had in my life? Now being diagnosed with bipolar, and adhd?
Meds for these do seem to be working but over the years being told i had depression and trying depression meds that made things much much worse was horrible. is it truely bipolar, adhd or is it from a tbi ??
Missy,
Of course no one can be certain on these matters without a careful evaluation, and without a better sense of the symptom nuances… but it is very common that TBI is missed, bipolar symptoms appear, as the appearance is bipolar, but the underlying issue is the TBI which needs direct attention from several other directions – most especially a specific nutritional and exercise program as well as the psych meds. Best results: Neurotransmitter measurements outlined on this NeuroScience page here. Download the pdfs there for specifics.
Be well!
cp
Dr. Parker I would like to ask a question..My son is now 15 and has been in and out of Behavioral Health for what we have been told is a mood disorder and ADHD. This is just the beginning. Two years ago while riding his bike, the front tire flew off and he was airborne knocking himself unconscious on the curb..He was life-flighted by helicopter and placed in ICU for three days with Traumatic Brain Injury with subdural hematoma….It seems that none of the Drs. want to address the brain injury and say it was not significant enough to warrant further looking into..I am so tired of hearing every problem he has is from a mood disorder, (severe mood swings that come on with no warning, last about 5-10 minutes and then everything is back to normal so to speak.) His sleep patterns are crazy and suffers terribly from insomnia. One could say that this does mimic bi-polar, but I don’t see any cycling…His mood swings are almost daily and come on with no warning…One other troubling symptom is he seems to have over sensitive senses. The sound and feeling of certain things just about send him over the edge. Is this a common symptom with TBI? I am getting very frustrated and not sure what to do to help him..Just wish someone would listen..I have made an appointment for him to have a complete neurological workup done with a neuro-psychiatrist am I headed in the right direction? Any suggestions that could help me and the family, as these mood swings are getting harder and harder to live with…Are there any meds that seem to show a promising effect for those that experience irritability and aggression? Please send me an e-mail back…..I need to hear something positive.
Lisa,
Your findings are, more regretfully, not uncommon, -as most with TBI at our local brain injury association have had similar experiences. On the psych side: “The psychs need to become,” as my Norfolk colleague Paul Aravich has commented “more involved with the brain, and the neurologists need to focus more on the mind.” Many don’t know what to do with brain injury, and the meds are often simply ‘bipolar limited,’ set up by the appearances of the surface/symptom function rather than the underlying brain problems. These folks often do look bipolar, and that is a shame – if the only tool you have is a hammer then everything looks like a nail.
Having said all of that you need to figure out what to do. The meds must be determined by a variety of things. We always, and I repeat, always, test TBI for biomarkers with neurotransmitters. See several articles here, and this CorePsych NeuroScience, neurotransmitter page for many more downloads on that subject. Supplements are a big part of recovery and this post on Brain Injury has a few tips on the supplement side.
Actually, I just don’t like to throw various meds, or supplements, or intuitively based neurotransmitter precursors – I am a strong advocate of measurement and precision. Find someone who can jump on this by simply interviewing folks until you find someone locally, or come over and see us – this is one of my favorite subjects.
cp
Dr. Parker, what type of tests or scans would you recommend to the Drs. when addressing the issues that I have brought to your attention on my sons behalf….Do you think the brain injury was significant enough to press the issue furthur than just an ADHD/ mood disorder diagnosis? He is currently taking Lamictal and Vyvanse both of which have shown no real significant improvement in his symptoms…Sincerely, Lisa
Lisa,
Such recommendations are difficult to make for those in denial or uniformed. Having done that many times I can tell you they will, as they already have, likely blow you off again. Best to find someone specializing in Post Concussive Syndrome, and look to connect with a local brain injury association, as they will have recommendations that will save you considerable time.
The next problem is getting the meds and supplements right – take a look at CorePsych Books for a book by Perlmutter called the Better Brain Book, it will have more specifics if you can’t find anyone.
cp
Dr. Parker,
At the age of 5 my son was diagnosed with ADHD and placed on medication. He repeated kindergarten the following year with the same teacher. That year he was hit head on by a truck sustaning closed head injury, 7th and 8th nerve brain stem injuries and a mild stroke. After years of fighting and doctors then trying to diagnose my son with Bipolar disorder, I finally had a neuropsych eval done that did show mild to moderate TBI.
Now we are persuing compensation and his teacher of the time says that he acted the same prior to the accident as he did the last 4 weeks of school after and his grades show no change, therefore did not have any symptoms of TBI. (Teachers are now medical experts? I am a teacher myself.) He has always been very intelligent and the TBI has not effected his grades. His behavior and emotionality, inhibitions and overall personality was greatly affected. The symptoms that came about after the accident grew worse over years and my son was placed inpatient behavior unit in which they wanted to diagose Bipolar and disregard the head injury.
My question is this, 8 years post accident, how do we prove the difference between an existing case of ADHD with the secondary condition of TBI?
Crystal
Crystal,
This question is one of the inevitable questions asked often with SPECT imaging results from accidents or injury. The teacher was commenting on but one of the brain facilities, intelligence. TBIs often have little effect on intelligence. While his challenges appear superficial or non existent, they can be dramatically limiting nevertheless… that’s why I call brain injury The Masquerader.
Forget Halloween, TBI can wear many disguises, many hats, and hide behind mysterious symptoms that have been overlooked by both professionals and the public for years. Only recently with SPECT and PET imaging have we been able to codify accurately specific metabolic functional impairments in brain activity. Neurospsychological testing has demonstrated changes for years, but the brain pictures will tell the jury exactly where the impairment resides.
The hard part, showing that the current condition was not preexisting the injury. For that you need to review as many parameters as possible with questionnaires before and after, – and review from observations before and after that would document mood dysregulation.
Use your local brain injury association for checklists, and focus as much a possible on the functional systems. I do recommend SPECT imaging for a difinitiive review of the specifics, and interestingly, insurance will often pay if the symptoms are compelling and recommended by an independent neurologist, or person not economically tied up with the SPECT process itself.
cp
Thank you so much for the advice. On the SPECT test, will the injury still show itself 8 years later? He has horrible migraines still, so I may have a way to get the referel with that. He is now off all medications, they just didnt help and actually made him feel worse. He was put on mood stabalizers and ADHD meds and after years it was evident to us that they had little to no effect. He works very hard to control what doctors wanted to control with meds. We have given up on finding help and decided to just work together as a family. It is hard and lonely at times. But our son is gifted, kind and so very smart. If you didnt know about his accident, you would find it hard to even guess that he suffers from TBI. It is just as exhausting for him as it is for us. We make so many mistakes. I often say that I could do a better job if it was a disability that I could see with my eyes every time I look at him, rather than a silent invader that makes us forget it is there.
Unfortunately, the burden of proof lies for me to show. And I dont know who to turn to for help in a clinical diagnosis. Once I mention that we are in litigation, most will retract their help in fear of being held accountable for the diagnosis. So, we have the diagnosis and no doctors or therapist in our area to treat it, let alone help us show the difference in the preexisting ADHD and the TBI to a jury. So we continue to research and work on it as a family.
I am always intersested in any and all information that experts such as yourself can pass on to me. Thank you so much for your time.
Crystal
Crystal,
Because you might be involved in litigation your interests will best be served offline… note to follow via email.
cp
Greetings Dr. Parker
We have a 9 year old boy who at the age of 3 sustained a direct impact to the backside of his head after falling from a 3-foot high stage. Factoring in his height at the time to about 2 feet or so, that would be equivalent to at least five feet. There was no loss of consciousness per se, and we did not seek medical or emergency care at the time. Hindsight is 20/20 and memories of our son as once being low-key and well-adjusted before the injury, somehow evolved post-event as difficult, volatile, and oftentimes, inconsolable. He has serious behavioral issues at school and has been a target for an ADHD diagnosis since first grade. We’ve been resistant because of our reluctance to medicate. The epiphany for a possible TBI connection just came recently this year. How do we go about acquiring proper testing in order to resolve this? Beginning to feel the pressure to code, we’ve become desperate for a diagnosis. For reasons previously outlined, the school agreed to a pediatric neurologist visit at our insistence. The visit may have been no longer than 20 minutes and he refused to test for anything TBI related! We plan to change pediatricians for a more holistic approach and to one who has a TBI background and experience. Your thoughts and suggestions would be most appreciated. I thank you in advance.
Sheila,
No doubt that this boy does deserve SPECT functional imaging to evaluate causes of dysfunction. This is a fairly typical history and I regularly see this in my office at least 4-5X/day. The public is longing for a tool to evaluate brain function explicitly – and SPECT does it – in spite of the multiple naysayers who don’t know how to use it, and have never experienced using it.
A concern does arise in the following regards. Many who do SPECT are turning out cookie cutter reports with ‘perhaps this and perhaps that’ as recommendations. Many do not wish to see [or follow patients], and evaluation reports are limited to the psych drugs that can be used to control behavior, – not the complete evaluation that a boy like this deserves in terms of nutrition, neurotransmitter dysfunction and . Many are more like nuclear med evaluation guys focused only on the report, ‘these are the findings, now let your docs decide what to do down the road.’ [Much less risk for missing the mark.]
Just to clarify for readers: As you may have guessed, having been reading these reports for years, I have a significantly different approach, covering considerably more bases in my evaluation, do use SPECT as part of a comprehensive eval, and then continue, if the person has been seen in my office, to chase down the best combination of interventions. SPECT itself is only the beginning of the process, brain injury issues and the multiple sequellae can take considerable time – more of a marathon than an expensive 100 yard dash.
Thanks for your question, best wishes for chasing down your next answers,
cp
Hello,
My name is Kimberley and I am in B.C. Canada
I was T-boned in my mini van at an intersection 3 years ago, and i was dazed confused and embarrassed, but fine otherwise…went home and slept for weeks day and night, I cried all the time and then became very depressed..I have since been diagnosed with P.T.S.D. anxiety disorder, panic attack disorder, major depressive disorder, and now seeing my 7th or 8th specialist/I hvae now also been diagnosed with bi polar disorder. I am quite concerned with drugs and what type will make me worse as i was put on effexor and that was very bad for me. I am wondering would a spect scan benifit me ? how? would i end up with yet more disorders? and how do I go about getting one?
Kimberley-
Without knowing the details of your situation I can tell you that SPECT is best used in the process of understanding many of the problems you list – especially if you have had a TBI. There are, however, many more options for the evaluation process, many more than simply SPECT, and many with much less cost. I will connect with you off line to better understand your challenges and discuss other options.
Thanks for reading this post-
cp
Adeline-
If you have no recurring problems, no problem. If you find yourself confused or having any symptoms that are unexplained, such as persistent headache your best interests would be served by a review in the ER or your doc.
cp
I fell and hit my head on a hollow door. The hit is on the left rear side of my head and raised a egg-size lump. I iced it down and this morning it is down but sore. My question is I have no side effects. How important is it to see my Dr. or have an MRI?
Thank you
Adeline
The first onset of problems beginning with depression was at 12 after being hit by a car at the same age. The onset of Fibromyalgia came after a car accident in 1992 (also about the time I was first diagnosed with ADHD). Maybe that all makes sense now!
Sibyl,
One of the important consequences of brain injury – the direct change to neurotransmitter function, and to rearrangement of neurotransmitter pathways is also overlooked.
Do sign up for email updates with the blog here, as I will be writing about neurotransmitter precursors and TBI soon. I have a small private study going on in my office with TBI and neurotransmitter consequences – and will keep you posted on that one as well.
And if you are refractory to meds… this whole picture makes much more sense.
cp
Dr. Parker,
I am a patient of yours and sustained a mild brain injury (if there is such a thing) in August of 2008. Without giving you a full run down, I was skateboarding, fell, fractured my skull, and was browning out for quite a few hours afterward (I was able to get up, stumble to my car, call a friend, immediately after the accident). The only residual effect I had (which has since ceased) was a fraction of a second of dizziness if I rolled over and stood up the wrong way (i.e. getting out of bed). CAT, Xray all checked out.
Do you think something like this would make me a candidate for a SPECT scan? As someone who’s generally interested in neuroscience as a hobby, I’ve never really had a medical reason to get this done but have always wanted to.
Think my insurance would cover it (BCBS Fed)? 🙂
(And, of course, could find some interesting info?)
-Josh
Josh,
Brain injury is clearly a reason for further evaluation with SPECT – the benefits are outlined here in this article: Why SPECT?
And frequent questions are answered here: SPECT FAQ
Let’s discuss this new development more at our next meeting.
cp
I wonder if meconium related stress during childbirth can cause or mimic TBI. Our son, who seems to be a moving target for a diagnosis (i.e. ADD, Depression, Bipolar, etc.) may have had some sort of brain injury when being born but this has never been addressed.
All I remember is the doctor while delivering the baby, said there was meconium and nothing else was ever mentioned.
Our son’s life appeared fairly normal, with very high intelligence until symptoms of ADD began appearing around third grade and depression around eighth. He is now a young adult and things are getting worse in spite of all the professional help he’s received through the years.
We’d like to do a SPECT scan to address this. What has been your experience with this type of situation?
Les,
SPECT is very useful in differentiating the TBI from or including the PFC changes with ADHD. ADHD shows often in the second grade and becomes more challenging with decreased structure as school progresses.
SPECT is the watershed for assessing brain function even if CAT and MRI have proven negative in the past.
cp